In order to maximize efficiency and minimize injury risk, cyclists have to optimize both machines at play, the two machines being the bike, and the cyclist.
Battling between the bike fitting and poor biomechanics of a cyclist is a recipe for pain and poor efficiency. The following is a list of common cycling injuries as well as the biomechanical flaws that may be causing them. Fixing the flaws with corrective exercises is only half the battle, as a poor fitted bike will contribute to these injuries as well.
1. Low Back Pain
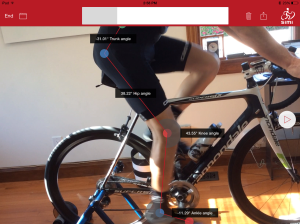
Number one, and probably the most common is low back pain. Just because you are sitting while riding, doesn’t mean you can relax and sit in a slumped posture. A slumped posture places excessive tensile force on the muscles in the low back, and asking those muscles to work extra hard for several miles usually results in some amount of discomfort. The main motion to look out for is a pelvis that is posteriorly tilted like this athlete in the picture below.
The posterior pelvic tilt is typically caused by decreased hip flexion, a motion often limited by tight hamstrings. Further, decreased abdominal strength can result in this slouched forward position. Have your therapist assess your hamstring length and your abdominal strength to determine if these may be the cause of the low back pain you are experiencing.
2. Hip Impingement
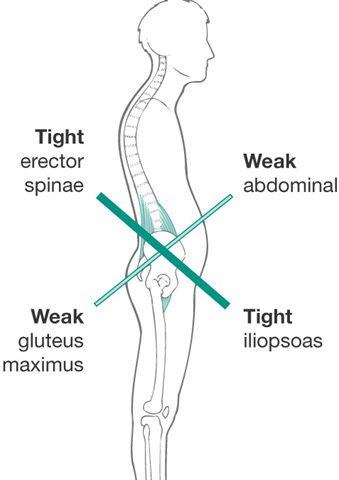
When the head of the femur pinches with the acetabulum of the pelvis a pain in the anterior aspect of the groin may occur. This pinching tends to occur when an individual places their hip into more flexion, adduction, and internal rotation than their hips actually have motion for. It can also occur due to weak, or inactive gluteal and abdominal muscles as their role is to rotate the pelvis posteriorly. Riding with your knee more medial than your hip can result in impingement at the hip, pain in the anterior aspect of your thigh, and definitely decreased efficiency while riding.

The excessive adduction and internal rotation can result in impingement at the femoral-acetabular joint.
3. Patello-femoral (Knee) Pain
The movement causes of anterior knee pain is very similar to the movement caused of hip impingement. The adduction and internal rotation of the femur causes impingement at the hip, as well as compression of the patella and femur at the anterior knee. The picture below shows how a simple step down test can identify this movement pattern, which suggests poor gluteal recruitment and / or strength.
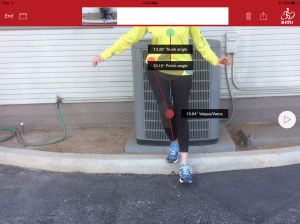
The excessive genu values during a step down may result in excessive compression at the patella-femoral joint.
4. Achilles Tendonitis
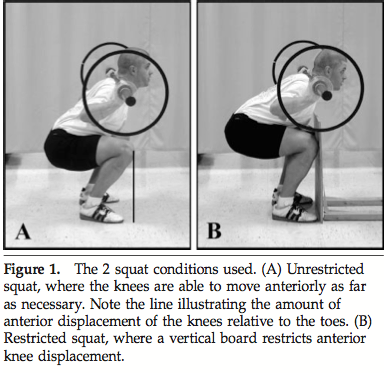
Posterior ankle pain while riding is often due to excessive plantar flexion of the ankle at the bottom of the power stroke. If you are pedaling with your toe pointed down at the bottom of the stroke, you are likely overusing your posterior ankle muscles which attach to the achilles. This overuse can lead to tendonitis. Reasons why this occurs can be a poor bike fitting where the seat may be too high, but it can also occur as a result of poor activation of more proximal musculature such as the gluteals and quadriceps.
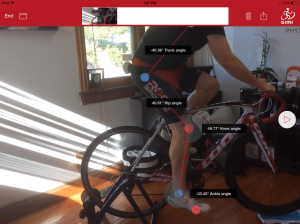
5. Neck Pain
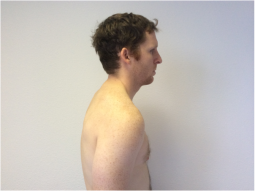
The amount of mid back curvature while cycling certainly can lead to higher stress at the cervical spine or neck as you keep your head up to see what is ahead of you. Excessive curvature (known as excessive thoracic kyphosis) will lead to an even greater stress at the cervical spine. As the picture below shows, the excessive kyphosis is often a result of limited hip flexion. This means that solving your neck pain while riding often means improving your hip ROM through stretching and improving abdominal control.
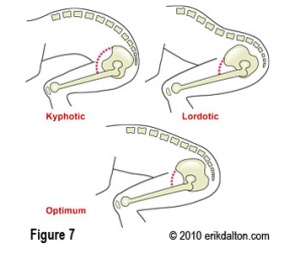
Excessive kyphosis at the thoracic spine can result in excessive compression at the cervical spine while cycling.
The first step to eliminating pain and improving efficiency on the bike is to diagnose the problem. Often times a bike fit and a movement assessment will identify the cause of the dysfunction. Our next blog post will focus on movement assessments and exercises you can start doing to treat the dysfunction and keep you riding.
In the meantime, check out www.optimalmovementpt.com for more cycling, movement, and corrective exercise ideas, or click here to schedule your movement assessment at Optimal Movement.