Welcome to the new Physical Therapy world. Gone are (or should be) the days of the ultrasound, hot pack, and nice massage. No longer do we treat only the location of pain. Each patient who fell through the cracks after their e-stim machine turned off begged for something more, and the time has certainly come.
Say hello to your new Physical Therapist. Your new therapist doesn’t bother dusting the ultrasound machine as he or she is too busy examining movement. One hour of pain free walking after short term treatments is not enough. Your new Physical Therapist is asking why the pain always comes back after one has sat for too long. A manipulation is only magical if the pain doesn’t return after repeated bending. Physical Therapists don’t simply stop at the area of pain, they move on to determine why that area of pain is under so much stress during seemingly simple movements.
Shooting numbness down your leg while sitting? Piercing pain at your low back with only minutes of walking? Could it be that the answer to your problem is not a laser to damaged areas of your spine? Could it be that the reason the pain occurs while you are sitting is due to tight hip musculature? What if stretching the hip flexors could relieve the pain associated with the osteoarthritis found on the x-ray? Some colleagues of mine have recently explores the relationship between hip stiffness and low back pain here.
In a nutshell, every movement is comprised from multiple parts of the body. Even sitting, the most common position for todays common man is quite complex. Sitting in a low seat requires up to 110 degrees of hip flexion. Ideally, the pelvis will not tilt posteriorly, and the low back will not round into flexion. Unfortunately, most people don’t have 110 degrees of hip flexion. Sitting without hip mobility can result in excessive tensile stress to the low back, and therefore cause that aching low back pain after prolonged sitting.
You can have soft tissue done, a manipulation, or even surgery if you can find the right (or wrong!) surgeon. But, when you go back to sitting without the hip flexibility the pain will return.
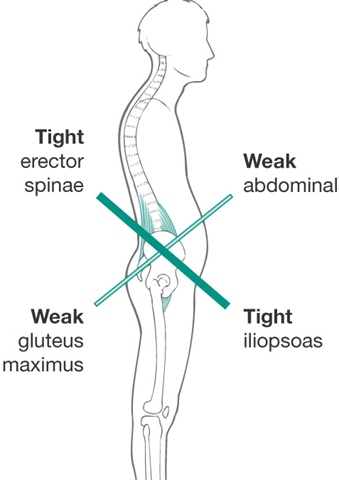
It works both ways. Some individuals have tight hip flexors and therefore lack full hip extension while walking. This results in excessive extension at the spine, and/or a compensatory rotation at the pelvis resulting in unneeded torque at the spine.
Once again, any treatment at the spine is missing the cause of the dysfunction.
The Physical Therapy world is changing. You can now see your physical therapist without a Physician prescription in most states. More and more therapists are screening movements and looking for this type of hip dysfunction well before the low back pain even starts. Find yourself a great local therapist and determine the cause of the pain today. Check http://www.optimalmovementpt.com for more information.
What are your favorite hip mobility exercises? Stay tuned for the next blog to learn the best mobility exercises for the hip.